
The emergence of long COVID, medically termed Post-Acute Sequelae of SARS-CoV-2 infection (PASC), has fundamentally transformed our understanding of viral recovery and rehabilitation medicine. Unlike traditional acute illnesses that follow predictable recovery trajectories, long COVID presents a complex, multisystem condition that demands innovative, patient-centered approaches to care and rehabilitation.
This comprehensive guide examines evidence-based strategies for supporting individuals experiencing persistent symptoms following COVID-19 infection, drawing from emerging research, clinical expertise, and patient experiences to provide practical frameworks for recovery. The rehabilitation journey for long COVID patients requires careful orchestration of medical intervention, lifestyle modification, and psychosocial support, recognizing that each patient’s experience is uniquely complex and deeply personal.
Understanding the Multisystem Nature of Long COVID
Long COVID affects virtually every organ system in the body, creating a constellation of symptoms that can fluctuate unpredictably and interact in complex ways. The condition challenges traditional medical models that typically address single-system disorders, requiring instead a holistic understanding of how interconnected physiological processes contribute to ongoing dysfunction.
The neurological manifestations of long COVID extend far beyond the commonly discussed “brain fog,” encompassing difficulties with executive function, working memory, processing speed, and emotional regulation. These cognitive changes can profoundly impact daily functioning, professional performance, and quality of life. Patients often describe feeling as though they are operating through a mental haze, struggling to find words, maintain concentration, or complete complex tasks that were previously effortless.
Cardiovascular complications represent another critical dimension of long COVID, with many patients experiencing persistent tachycardia, exercise intolerance, chest pain, and blood pressure irregularities. The heart’s response to physical and emotional stress becomes dysregulated, creating a cascade of symptoms that can be mistaken for anxiety or deconditioning when, in fact, they represent genuine physiological dysfunction requiring careful medical management.
Respiratory symptoms persist in many long COVID patients, even those who experienced relatively mild acute infections. Shortness of breath, cough, and reduced exercise tolerance can significantly limit daily activities and contribute to deconditioning cycles that further compromise recovery. The respiratory system’s healing process appears to be prolonged and complicated in many patients, requiring specialized rehabilitation approaches.
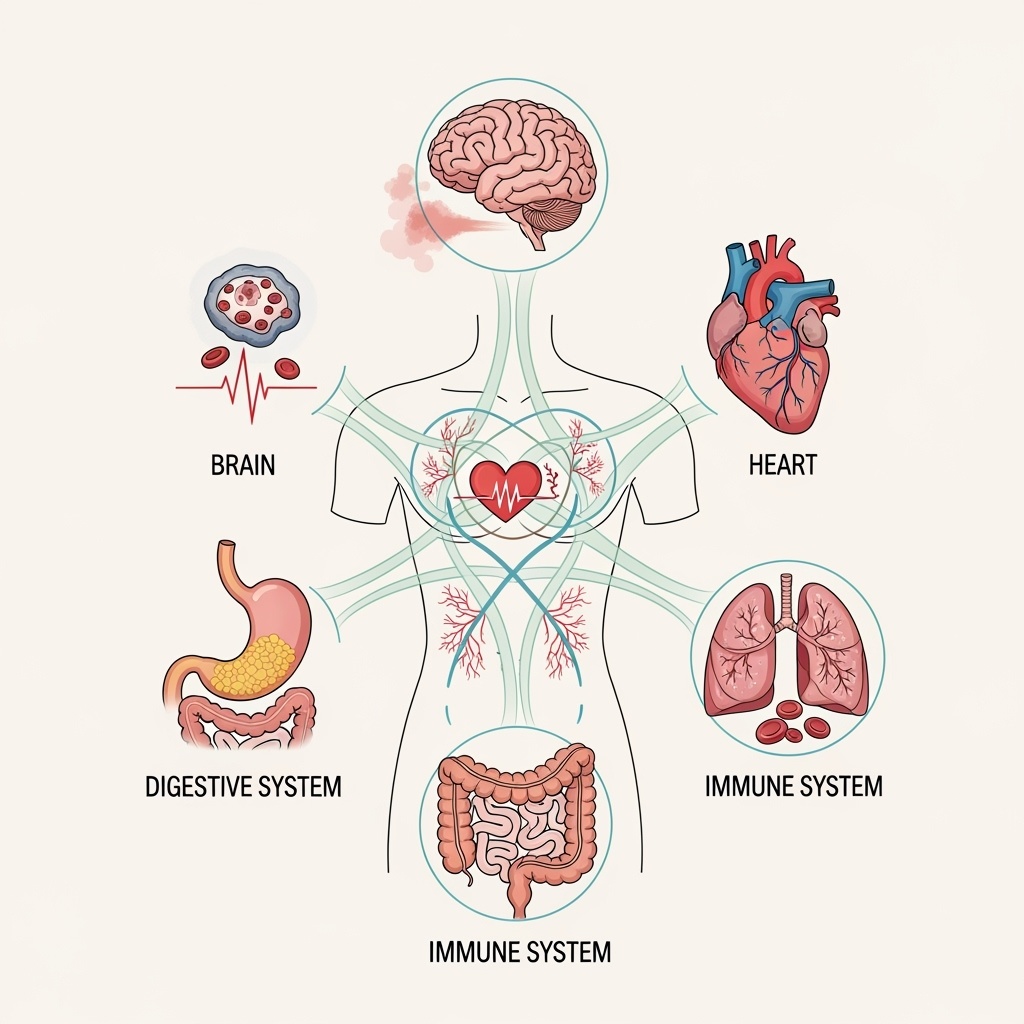
The gastrointestinal manifestations of long COVID often receive less attention but can be equally debilitating, including persistent nausea, altered taste and smell, digestive dysfunction, and food intolerances. These symptoms can complicate nutritional rehabilitation and contribute to fatigue and weakness cycles that impede overall recovery progress.
Post-Exertional Malaise: The Central Challenge in Long COVID Rehabilitation
Post-exertional malaise (PEM) represents perhaps the most critical concept in long COVID rehabilitation, fundamentally distinguishing this condition from typical post-viral fatigue or deconditioning. PEM is characterized by a disproportionate worsening of symptoms following physical, cognitive, or emotional exertion that can be delayed by hours or days and may persist for extended periods.
Traditional rehabilitation approaches that emphasize graded exercise therapy or progressive activity increases can be counterproductive and potentially harmful for patients experiencing PEM. Instead, rehabilitation must be carefully calibrated to respect the body’s current capacity while gradually and safely expanding tolerance for activity. This requires sophisticated assessment of individual energy reserves and careful monitoring of symptom responses to various types of exertion.
The concept of “energy envelope theory” becomes central to successful long COVID rehabilitation. Patients must learn to identify their current energy capacity on any given day and plan activities accordingly, avoiding the boom-bust cycles that can perpetuate and worsen symptoms. This approach requires developing acute self-awareness and accepting limitations that may fluctuate unpredictably.
Pacing strategies form the foundation of effective PEM management, involving the careful distribution of activities throughout the day and week to prevent symptom exacerbation. Patients learn to break tasks into smaller components, incorporate regular rest periods, and modify activities to reduce their physiological and cognitive demands. This approach requires significant lifestyle adjustments and often challenges deeply held beliefs about productivity and achievement.
Cognitive Rehabilitation and Neurological Recovery
The cognitive effects of long COVID require specialized rehabilitation approaches that address both the underlying neurological dysfunction and the practical challenges of daily cognitive demands. Cognitive rehabilitation begins with comprehensive assessment to identify specific areas of impairment and preserved abilities, providing a foundation for targeted intervention strategies.
Memory rehabilitation techniques focus on both compensatory strategies and direct cognitive training. Patients learn to use external memory aids effectively, develop organizational systems that reduce cognitive load, and practice memory strengthening exercises appropriate to their current capacity. The goal is not necessarily to restore pre-illness cognitive function but to maximize current abilities and develop workarounds for persistent deficits.
Attention and concentration difficulties require multifaceted approaches that address both focused attention and divided attention challenges. Patients practice attention training exercises, learn environmental modifications that reduce distractions, and develop strategies for managing cognitive fatigue. These interventions must be carefully dosed to avoid overwhelming already compromised cognitive resources.
Executive function rehabilitation addresses planning, problem-solving, and decision-making difficulties that can significantly impact independence and quality of life. Patients learn to break complex tasks into manageable steps, use decision-making frameworks that reduce cognitive burden, and develop routines that minimize the need for constant executive decisions. This work often involves significant life restructuring to accommodate cognitive limitations while maintaining meaningful engagement in valued activities.
Cardiovascular Rehabilitation and Exercise Physiology
Cardiovascular rehabilitation for long COVID patients requires careful modification of traditional cardiac rehabilitation principles to accommodate the unique challenges of post-viral cardiovascular dysfunction. The approach must balance the benefits of cardiovascular conditioning with the risks of symptom exacerbation and PEM.
Heart rate monitoring becomes essential for safe exercise prescription, with many patients requiring modified target heart rate zones that account for dysautonomia and altered cardiovascular responses. Traditional age-predicted maximum heart rate formulas may be inappropriate, necessitating individualized assessment of cardiovascular responses to exertion.
Exercise prescription begins with very low-intensity activities that can be performed within the patient’s current tolerance, gradually progressing only when symptoms remain stable or improve. This may mean starting with seated exercises, short walks, or gentle stretching routines that would seem trivial for healthy individuals but represent appropriate challenges for deconditioned long COVID patients.
Orthostatic intolerance and postural orthostatic tachycardia syndrome (POTS) symptoms require specific interventions including compression garments, increased fluid and salt intake, and graduated position changes. Patients learn to monitor their cardiovascular responses to position changes and implement strategies to minimize symptoms during daily activities.
| Cardiovascular Rehabilitation Phases | Duration | Activities | Heart Rate Target |
| Phase 1: Stabilization | 2-4 weeks | Seated exercises, breathing techniques, gentle stretching | Below anaerobic threshold |
| Phase 2: Foundation Building | 4-8 weeks | Short walks, recumbent cycling, light resistance bands | 60-70% of individualized maximum |
| Phase 3: Progressive Conditioning | 8-16 weeks | Increased duration activities, varied exercise types | 70-80% with symptom monitoring |
| Phase 4: Functional Integration | Ongoing | Sport-specific or activity-specific training | Individualized based on goals |
Respiratory Rehabilitation and Breathing Techniques
Respiratory rehabilitation for long COVID addresses both the physical limitations in lung function and the dysfunctional breathing patterns that often develop in response to persistent respiratory symptoms. The approach combines traditional pulmonary rehabilitation techniques with specialized interventions for post-viral respiratory dysfunction.
Breathing pattern retraining addresses the hyperventilation and inefficient breathing patterns that commonly develop in long COVID patients. Patients learn diaphragmatic breathing techniques, paced breathing exercises, and breath control strategies that improve respiratory efficiency while reducing the work of breathing. These techniques often provide immediate symptom relief and serve as foundation skills for other rehabilitation activities.
Respiratory muscle training using inspiratory muscle trainers or resistive breathing devices can help address respiratory muscle weakness and improve overall respiratory function. However, these interventions must be carefully prescribed and monitored to avoid respiratory muscle fatigue that could worsen symptoms.
Airway clearance techniques become important for patients with persistent productive cough or chest congestion. Patients learn various techniques for mobilizing secretions and maintaining clear airways while avoiding excessive coughing that can lead to symptom exacerbation.
Exercise-based respiratory rehabilitation focuses on improving respiratory endurance and efficiency through carefully graded activities that challenge the respiratory system without causing significant symptom flare-ups. This often involves interval training approaches that allow for recovery periods between exertion phases.
Nutritional Rehabilitation and Metabolic Support
Nutritional rehabilitation plays a crucial role in long COVID recovery, addressing both the direct effects of the illness on nutritional status and the metabolic dysfunction that can persist long after acute infection. Many patients experience significant changes in appetite, taste, smell, and digestive function that complicate nutritional rehabilitation efforts.
The inflammatory nature of long COVID often increases nutritional needs while simultaneously impairing nutrient absorption and utilization. Patients may require higher protein intake to support tissue repair and immune function recovery, but gastrointestinal symptoms can make achieving adequate nutrition challenging. This creates a complex situation requiring individualized nutritional strategies.
Micronutrient deficiencies are common in long COVID patients and may contribute to persistent fatigue, cognitive dysfunction, and immune system abnormalities. Comprehensive nutritional assessment often reveals deficiencies in vitamin D, B vitamins, iron, zinc, and other nutrients essential for optimal physiological function. Targeted supplementation, when appropriate, can support recovery processes.
Anti-inflammatory nutrition approaches focus on reducing systemic inflammation through dietary modifications that emphasize omega-3 fatty acids, antioxidant-rich foods, and minimally processed whole foods. These dietary changes may help modulate the ongoing inflammatory response that characterizes long COVID while supporting overall health and recovery.
The timing and composition of meals become important considerations for patients experiencing blood sugar instability, digestive dysfunction, or energy fluctuations throughout the day. Patients learn to eat in ways that support stable energy levels and minimize symptom exacerbation related to blood sugar swings or digestive distress.
Sleep Rehabilitation and Circadian Rhythm Restoration
Sleep disturbances are nearly universal among long COVID patients and often represent both a symptom of the condition and a significant barrier to recovery. Sleep rehabilitation requires addressing multiple factors that contribute to poor sleep quality, including pain, anxiety, breathing difficulties, and circadian rhythm disruption.
Sleep hygiene education forms the foundation of sleep rehabilitation, helping patients create optimal sleep environments and develop consistent bedtime routines that support natural sleep processes. However, traditional sleep hygiene recommendations may need modification for long COVID patients who experience unpredictable symptom fluctuations that can disrupt sleep patterns.
Circadian rhythm restoration techniques help patients reestablish healthy sleep-wake cycles that may have been disrupted during acute illness or through prolonged periods of reduced activity and light exposure. Light therapy, timed activities, and structured daily routines can help reset disrupted circadian rhythms and improve sleep quality.
Pain and discomfort management strategies are essential for patients whose sleep is disrupted by persistent physical symptoms. This may involve positioning techniques, heat and cold therapy, gentle movement, or relaxation strategies that reduce symptom severity during nighttime hours.
Anxiety and hypervigilance often interfere with sleep initiation and maintenance in long COVID patients who may have developed heightened awareness of bodily sensations or fears about symptom worsening during sleep. Cognitive-behavioral techniques and relaxation training can help address these psychological barriers to restorative sleep.
Psychological Rehabilitation and Mental Health Support
The psychological impact of long COVID extends far beyond the direct neurological effects of the virus, encompassing grief over lost abilities, uncertainty about recovery, social isolation, and the challenges of navigating medical systems that may not fully understand or validate the patient’s experience.
Grief counseling helps patients process the multiple losses associated with long COVID, including loss of physical abilities, cognitive function, social roles, and future plans. This grief process is often complicated by the uncertain and fluctuating nature of symptoms, making it difficult to achieve acceptance or closure. Patients benefit from support in recognizing and validating their grief while developing coping strategies for ongoing uncertainty.
Anxiety management becomes crucial for patients who develop heightened health anxiety, fear of symptom recurrence, or panic responses to physical sensations. Cognitive-behavioral techniques help patients develop more balanced thinking patterns about their symptoms while learning practical strategies for managing anxiety when it arises. Exposure therapy approaches may be modified to help patients gradually resume activities they have been avoiding due to fear of symptom exacerbation.
Depression screening and treatment address the complex relationship between neurobiological changes from COVID-19, the psychological impact of chronic illness, and the social consequences of functional limitations. Treatment approaches must account for the fact that depressive symptoms may result from both psychological responses to illness and direct neurological effects of the virus.
Social skills rehabilitation helps patients navigate changed relationships and social expectations while managing an invisible chronic illness. Patients learn communication strategies for explaining their limitations to family, friends, and employers while advocating for appropriate accommodations and support.
Occupational Rehabilitation and Return-to-Work Support
Occupational rehabilitation for long COVID patients requires careful assessment of cognitive and physical demands in work environments, modification of job tasks and schedules, and collaboration with employers to develop sustainable return-to-work plans. The unpredictable nature of long COVID symptoms creates unique challenges for traditional vocational rehabilitation approaches.
Job analysis and modification involve breaking down work tasks to identify those that may be particularly challenging for long COVID patients and developing strategies for modifying or redistributing these responsibilities. This may involve changes to computer work patterns to address cognitive fatigue, modification of physical demands to accommodate exercise intolerance, or restructuring of work schedules to allow for rest periods and medical appointments.
Accommodation strategies help patients and employers identify workplace modifications that can support successful job performance while managing long COVID symptoms. These might include flexible work schedules, work-from-home options, modified job duties, additional break periods, or changes to the physical work environment. The key is finding accommodations that genuinely support the patient’s needs without creating undue burden for employers.
Graduated return-to-work planning recognizes that many long COVID patients cannot immediately resume full work responsibilities and benefit from phased return approaches. This might involve starting with reduced hours or responsibilities and gradually increasing demands as tolerated. The plan must remain flexible to accommodate symptom fluctuations and setbacks.
| Return-to-Work Phase | Duration | Work Capacity | Accommodations Needed |
| Assessment Phase | 1-2 weeks | N/A | Comprehensive functional assessment |
| Initial Return | 2-4 weeks | 25-50% capacity | Reduced hours, modified duties, frequent breaks |
| Gradual Increase | 4-8 weeks | 50-75% capacity | Flexible scheduling, task modification |
| Full Integration | 8+ weeks | 75-100% capacity | Ongoing accommodations as needed |
Family and Caregiver Support Systems
The rehabilitation of long COVID patients extends beyond the individual to encompass family members and caregivers who play crucial roles in supporting recovery while managing their own stress and adaptation challenges. Family-centered rehabilitation approaches recognize that the entire family system is affected by chronic illness and benefits from coordinated support.
Caregiver education helps family members understand the nature of long COVID, its effects on the patient, and how they can best provide support without enabling overdependence or contributing to symptom exacerbation. Caregivers learn to recognize signs of PEM, understand pacing principles, and support the patient’s rehabilitation efforts while maintaining appropriate boundaries.
Communication training helps families develop effective ways of discussing symptoms, limitations, and needs while avoiding patterns that might increase stress or conflict. Families learn to balance concern and support with encouragement of independence and self-management. This often requires significant adjustment of family roles and expectations.
Caregiver stress management addresses the significant burden that caring for a family member with long COVID can create. Caregivers benefit from their own support networks, stress management techniques, and respite opportunities that allow them to maintain their own health and well-being while providing support.
Family therapy or counseling can help address relationship changes, communication difficulties, and adjustment challenges that commonly arise when chronic illness affects family systems. Professional support helps families navigate these changes while maintaining healthy relationships and effective support patterns.
Technology Integration in Long COVID Rehabilitation
Modern rehabilitation increasingly incorporates technology solutions that can support long COVID patients in managing their symptoms, tracking their progress, and accessing care remotely. These technological tools must be carefully selected and implemented to provide genuine benefit without adding unnecessary complexity or stress to already overwhelmed patients.
Symptom tracking applications help patients monitor their symptoms, energy levels, and activity patterns to identify triggers, track progress, and communicate effectively with healthcare providers. However, these tools must be user-friendly and not so complex that they become another source of stress or cognitive burden for patients with cognitive limitations.
Wearable devices can provide objective data about heart rate, sleep patterns, activity levels, and other physiological parameters that inform rehabilitation planning and safety monitoring. The key is selecting devices that provide clinically useful information without overwhelming patients with excessive data or creating obsessive monitoring behaviors.
Telehealth platforms enable access to specialized long COVID care and rehabilitation services that may not be available locally. These platforms must be accessible to patients with cognitive limitations and technical difficulties while providing secure, high-quality care delivery. The technology should enhance rather than complicate the therapeutic relationship.
Virtual reality and digital therapeutics represent emerging areas of potential benefit for long COVID rehabilitation, offering innovative approaches to cognitive rehabilitation, stress management, and graded exposure therapy. However, these interventions require careful evaluation for appropriateness and effectiveness in the long COVID population.
Building Sustainable Recovery Programs
Long COVID rehabilitation requires sustainable approaches that patients can maintain long-term while adapting to changing symptoms and life circumstances. The goal is not necessarily to return patients to their pre-illness state but to help them achieve their optimal level of function and quality of life within their current limitations.
Personalized rehabilitation plans must account for individual differences in symptoms, severity, recovery patterns, and life circumstances. What works for one long COVID patient may be entirely inappropriate for another, requiring highly individualized approaches to care planning and implementation. This personalization extends beyond medical interventions to encompass lifestyle modifications, social support needs, and personal goals and values.
Progress monitoring systems help track rehabilitation outcomes while remaining flexible enough to accommodate the fluctuating nature of long COVID symptoms. Traditional rehabilitation outcome measures may not capture the subtle but important changes that occur in long COVID recovery, necessitating the development of more sensitive and relevant assessment tools.
Long-term maintenance strategies recognize that long COVID rehabilitation is often an ongoing process rather than a time-limited intervention. Patients benefit from developing sustainable self-management skills, ongoing professional support relationships, and flexible rehabilitation programs that can be intensified or modified as symptoms change over time.
Community integration remains a crucial goal of long COVID rehabilitation, helping patients maintain meaningful social connections and valued activities despite persistent limitations. This may require creative approaches to participation modification and social role adaptation while preserving personal identity and life satisfaction.
The future of long COVID rehabilitation lies in continued research into effective interventions, development of specialized care programs, and integration of patient experiences into evidence-based practice. As our understanding of this complex condition evolves, rehabilitation approaches must remain flexible and responsive to new knowledge while maintaining focus on patient-centered, holistic care that addresses the full spectrum of long COVID’s impact on human health and functioning.
Recovery from long COVID is possible, though it may look different than expected and require patience, persistence, and comprehensive support. The rehabilitation journey demands courage from patients, creativity from providers, and commitment from support systems, but the potential for meaningful improvement and adaptation offers hope for millions of individuals affected by this challenging condition.

